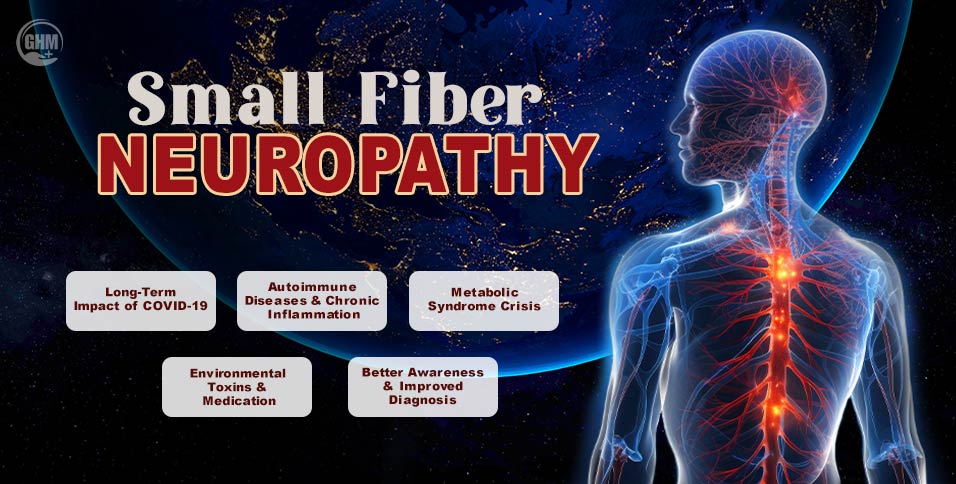
Small fiber neuropathy is increasingly being diagnosed across the world, raising concern among patients, families, and healthcare professionals. Once considered rare, this nerve disorder now appears more often in clinics. It currently affects 15 to 20 million adults over age 40 in the U.S. alone. It specifically affects older adults, people with chronic conditions, and those recovering from COVID-19.
Small fiber neuropathy affects the body’s smallest nerve fibers. These fibers control pain, temperature, and automatic functions like heart rate and digestion. Large nerves handle muscle strength, while small fibers transmit pain signals and regulate involuntary body functions.
As global lifestyles change and post-viral conditions increase, multiple factors drive this rise.
Therefore, this article explains why small fiber neuropathy cases are growing, what symptoms to watch for, and how early awareness protects nerve health.
Reasons Behind A Global Rise in Small Fiber Neuropathy
The prevalence of small fiber neuropathy has steadily increased over the last two decades. A long-term U.S. population study found rates rising to over 13 per 100,000 people. Meanwhile, European data suggests rates may exceed 50 per 100,000 in certain regions.
Experts agree that this trend stems from a combination of modern health challenges rather than a single source.
1. The Long-Term Impact of COVID-19
One of the strongest contributors is long COVID. This condition drives new cases of neuropathy through immune-triggered damage, months after the initial infection. Studies indicate that 46% of patients with painful post-acute sequelae of COVID-19 have biopsy-proven nerve damage.
2. The Metabolic Syndrome Crisis
Modern lifestyles are a primary driver of the risk of nerve damage. Metabolic issues cause chronic inflammation and reduced blood flow to nerves. Study shows roughly 51% of SFN patients also have diabetes.
- Diabetes: Increases the risk of SFN by 3.8 times.
- Obesity: Correlates strongly with nerve fiber loss.
- Hypertriglyceridemia: High fat levels in the blood contribute to nerve decay.
3. Vitamin Deficiency and Nutritional Gaps
Nutritional imbalances, particularly vitamin deficiencies like B12, remain silent contributors. Poor diets and gastrointestinal disorders often prevent the body from maintaining healthy nerve coatings. Addressing these gaps early is vital for prevention.
4 Autoimmune Diseases and Chronic Inflammation
Chronic inflammation from autoimmune diseases accounts for nearly 30% of diagnosed cases. Conditions like Sjögren’s syndrome and lupus are found in approximately 28% of studied SFN cases. In these cases, the immune system mistakenly attacks nerve fibers.
5. Environmental Toxins and Medication
Exposure to heavy metals and certain chemotherapy drugs can damage delicate fibers. As cancer survival rates improve, more patients live with treatment-related nerve disorders, as studies confirm that chemotherapy-induced damage is a growing public health concern. Exposure to heavy metals and pesticides can also contribute to these triggers.
6. Better Awareness and Improved Diagnosis
Finally, the rise is partly due to better technology, which gives precise detection and results. Clinicians now use skin biopsies and QSART (sweat tests) more frequently. Increased awareness means fewer people are misdiagnosed, unmasking “hidden” cases of this nerve disorder.
Common Symptoms To Watch For
1. Sensory Symptoms
- Burning or Stabbing Pain: Often starts in the feet.
- Allodynia: Extreme pain from light touches, such as clothing or bedsheets.
- Pins and Needles: Tingling that typically ascends in a “stocking-glove” pattern.
- Night Worsening: Pain intensity frequently peaks during late hours.
2. Autonomic Symptoms
- Dizziness: Feeling faint upon standing due to blood pressure shifts.
- Digestive Issues: Constipation or bladder dysfunction.
- Sweating Changes: Either excessive sweating or a total lack of sweat.
- Dryness: Persistent dry eyes or mouth.
These symptoms often appear gradually, which should not be ignored if they persist.
How Small Fiber Neuropathy Is Diagnosed in 2026
Modern diagnosis focuses on precision. Because standard EMG tests only check large fibers, they often appear normal in SFN patients.
- Skin Punch Biopsy: This remains the gold standard for counting nerve endings.
- QSART: A test to measure sweat response and autonomic function.
- Autonomic Testing: This measures sweat production and heart rate changes.
- Blood Panels: These check for vitamin levels and autoimmune markers.
Can Small Fiber Neuropathy Be Treated and Managed
While some cases of neuropathy are managed through multidisciplinary teams, treatment is often cause-specific.
While no universal cure exists, treatment focuses on three main goals. First, doctors manage underlying causes like diabetes. Second, they work to reduce daily pain. Third, they aim to slow further nerve damage.
Common approaches include medications like gabapentin, lifestyle adjustments, and immunotherapy. Early diagnosis greatly improves patient outcomes and long-term mobility.
You can take preventive steps to reduce risk factors:
- Maintain a healthy blood sugar level.
- Adopt a Mediterranean diet to manage weight and inflammation.
- Schedule annual screenings if you are obese or have diabetes.
- Monitor symptoms closely after viral infections like COVID-19.
End Note
The 2026 uptick in small fiber neuropathy underscores a global urgency for better metabolic control and post-viral vigilance. Understanding why the nerve condition is rising worldwide empowers individuals to seek timely care. As medical awareness grows, early intervention will help reduce long-term damage and improve global quality of life.
Did you find this information helpful? Share this article with your friends and family to help spread awareness about nerve health!
Sanskruti Jadhav
Frequently Asked Questions (FAQ)
- What makes small fiber neuropathy different from other nerve disorders?
It affects pain and autonomic nerves rather than muscle strength. This makes symptoms harder to detect with traditional strength tests.
- Is small fiber neuropathy linked to aging?
Risk increases as we age, but younger adults frequently develop it after infections or autoimmune flares.
- Can COVID-19 permanently damage small nerve fibers?
Yes. Evidence suggests long COVID can cause persistent damage that requires specialized neurological care.
- Is Neuropathy life-threatening?
It is rarely life-threatening, but it can severely diminish your quality of life if you leave it untreated.
- Can nerve damage be reversed?
Some cases improve significantly when you treat the underlying cause early enough.