In the intricate world of healthcare policy and clinical practice, Dr. William H. Tettelbach is a master navigator. As a top physician, executive, and president of the nation’s leading professional wound care association, he is waging a meticulous, evidence-based campaign to heal not just patients, but the very system designed to care for them.
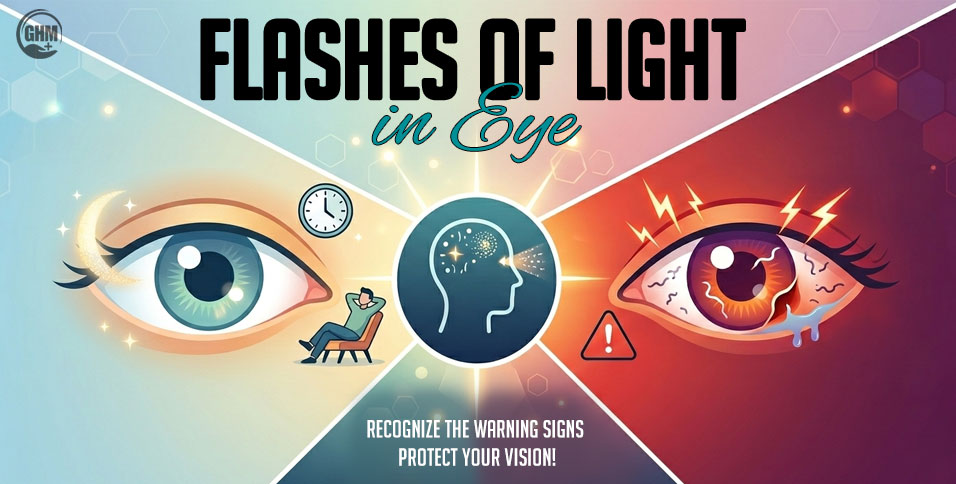
There is a silent epidemic in America, one that unfolds not in dramatic outbreaks, but in the quiet suffering of millions. It’s the epidemic of the chronic wound—the diabetic foot ulcer that refuses to heal, the vascular lesion that deepens, the persistent injury that can lead to amputation and a diminished life. According to the National Institutes of Health, 6.5 million people in the US suffer from chronic wounds—and the agency expects that number to increase. This is not a glamorous field of medicine. It is a complex, often frustrating landscape where biology, technology, and bureaucracy collide. And it is the world that Dr. William H. Tettelbach has dedicated his life to reshaping.
To meet Dr. Tettelbach is to encounter a mind that operates on multiple frequencies at once. He is a molecular biologist by training, an infectious disease specialist by practice, and a health economist by necessity. As the Chief Medical Officer at RestorixHealth, he oversees clinical strategy for more than 260 wound and hyperbaric centers. As the President of the American Professional Wound Care Association (APWCA), he is a central figure in shaping national policy. He speaks with equal fluency about the intricacies of cellular tissue products and the complexities of Medicare reimbursement models.
However, beneath the formidable titles and the encyclopedic knowledge is a core principle, a guiding belief that animates his entire career: “The best care begins with listening.” In a field increasingly driven by data, Dr. Tettelbach is a fierce advocate for the power of empathy. His life’s work is a testament to the idea that to truly fix a broken system, you must first listen to the needs of the patients it fails and the clinicians who struggle within it. He is not just a doctor; he is a systems-level diagnostician, and the system he is working to heal is one that affects the most vulnerable among us.
The Molecular Biologist’s Mission
Dr. Tettelbach’s journey into the specialized world of wound care was a gradual convergence of disciplines. It began at Vanderbilt University with a B.S. in Molecular Biology, a foundation that gave him a granular understanding of the building blocks of life. He earned his Doctor of Medicine from the University of Tennessee, followed by a residency in Internal Medicine and a demanding fellowship in Infectious Diseases at the University of Utah. It was here, at the intersection of complex diseases and patient care, that his mission began to crystallize.
“Early in my career, I became acutely aware of the challenges faced by patients with chronic wounds, particularly those with diabetes and vascular disease,” he recalls. He saw firsthand the devastating downstream effects—the cycle of infection, the threat of amputation, the loss of independence.
The statistics are stark. “If a patient with diabetes undergoes a non-traumatic lower-extremity major amputation, like a below-the-knee amputation, that patient’s five-year mortality rate increases to 50%,” Dr. Tettelbach notes. “Studies show that the five-year mortality rate for patients with chronic diabetic foot ulcers alone can be as high as 30%, which is similar to the mortality rate of certain types of cancer.” This awareness ignited a “passion for optimizing healing, reducing amputations, and improving patient outcomes.”
This passion led him to pursue specialized training in wound care, hyperbaric medicine, and medical informatics, a trifecta of skills that would become his signature. He took on the role of Program Director for the Duke University Undersea and Hyperbaric Medicine Fellowship program based in Salt Lake City, where he began mentoring the next generation of physicians. It was a career path defined by continuous learning, a transition from the academic to the corporate and from clinical practice to executive leadership, all in service of solving the multifaceted problem of the non-healing wound.
The President’s Vision
As President of the American Professional Wound Care Association (APWCA), Dr. Tettelbach now helms one of the most influential bodies in his field. His vision is not merely to maintain standards, but to build a more cohesive and powerful community. He champions a “multidisciplinary, inclusive, and forward-thinking” approach, a vision recently bolstered by the integration of the American College of Hyperbaric Medicine under the APWCA umbrella. This is a crucial step in addressing a core challenge of the field: that wound care is currently filled with dedicated clinicians from various specialties, such as general surgeons, podiatrists, and infectious disease specialists, who often lack standardized training specifically focused on wound care.
Dr. Tettelbach understands that clinical excellence alone is not enough. To truly move the needle, the APWCA must be a force for policy change. This understanding led to a crucial collaborative alliance with the Wound and Hyperbaric Association (WHA), a 501(c)(4) government affairs organization. This partnership gives the APWCA a powerful voice in Washington D.C., allowing them to advocate for sustainable reimbursement, regulatory reform, and equitable access to care. “Our mission includes championing science-based therapies, interdisciplinary collaboration, and meaningful engagement with policymakers,” Dr. Tettelbach asserts, “to ensure that patients receive the right treatment, at the right time, in the right setting.”
The Architect of Policy
When you ask Dr. Tettelbach about the most pressing challenges in wound care, he provides a clear, systemic diagnosis. The problems are not just clinical; they are structural. He points to “inconsistent reimbursement policies, lack of standardized clinical guidelines across institutions, and the underutilization of evidence-based therapeutic pathways.” These issues are compounded by the fact that wound care is not a recognized board-certified specialty. As he explains, not having a dedicated taxonomy or specialty code creates significant hurdles for funding and prevents many hospitals from seeing wound care as a true specialty that needs to be established and supported within their systems.
Dr. Tettelbach’s prescription for these systemic ills is specific and bold. He is a leading advocate for developing better-designed coverage determinations for key therapies like cellular and tissue-based products (or CAMPs, as they are known in the field). A thoughtfully crafted national coverage determination (NCD) could help create a uniform standard of care, ensuring equitable access for patients nationwide.
He is also championing a move away from “out of control” Average Sales Price (ASP) models for these products, arguing for a transition to fixed-fee reimbursement. This, he explains, would simplify billing, reduce the risk of fraud, and create the financial predictability needed for sustainable patient access while protecting the longevity of the Medicare trust fund.
These are not small changes. They represent a fundamental rewiring of the financial and regulatory structures of wound care. Reversing proposed reimbursement cuts and advancing these new models requires a deft political touch, an ability to build coalitions, and an unwavering reliance on data-driven advocacy. It’s a battle he has been waging for years, relying on collaboration and mentorship to navigate the labyrinthine structures of healthcare policy.
The Chief Medical Office’s Playbook
At RestorixHealth, Dr. Tettelbach translates his national policy vision into ground-level clinical reality. As Chief Medical Officer and a member of the executive team, he oversees the clinical strategy and quality outcomes for a network of over 260 hospital-affiliated wound care centers. His role is to ensure that the care delivered in a clinic in Florida is as evidence-based and effective as the care in a center in California.
He does this by standardizing clinical protocols, advancing data-driven decision-making, and championing research initiatives within the RestorixHealth network. This includes incorporating innovations that have pushed the field forward.
“The data published over the last couple of decades, for instance, have shown that the more one debrides a chronic wound—say surgically, with a scalpel—the quicker it heals,” Dr. Tettelbach notes, explaining that better outcomes are achieved when debridement is performed more routinely. He also champions new devices, from those that can quantify biofilm in a wound to direct more effective debridement, to portable near-infrared technology that images a wound to give clinicians a better understanding of tissue oxygenation.
This work is a massive undertaking that requires aligning the care delivery model with the national trend toward value-based healthcare, where payment is tied to quality outcomes rather than the volume of services. Dr. Tettelbach’s work at RestorixHealth is a living laboratory for the policies he advocates for on the national stage, proving that high standards and positive outcomes are not just possible, but scalable.
Accolades and Advocacy
Dr. Tettelbach’s work has earned him significant international recognition. He received the 2020 JWC Gold Medal for research contributions and, more recently, two 2025 Silver Medals from the same organization for excellence related to cellular and acellular products. His manuscript on the topic was named the Best of the Year at the 2025 CAMP Wound Care Summit.
These awards are more than just personal honors; they are currency in the world of advocacy. His publications, such as a recent cost-effectiveness analysis on CAMPs in Medicare, have directly influenced national debates. Being named President of the APWCA and serving on the CMS Advisory Panel are not just milestones; they are platforms. They amplify his voice and lend weight to his arguments, allowing him to push for the systemic changes he believes are so critical.
Looking to the future, Dr. Tettelbach’s focus remains sharp. He is committed to advancing the fixed-fee policy reform for CAMPs and is actively exploring the expansion of wound care access through mobile and digital health platforms. He is also dedicated to global health outreach, participating in annual medical missions in the Kingdom of Tonga.
When he steps away from the immense pressures of his professional life, he finds his balance in nature. He is an avid fisherman, pursuing his hobby everywhere from mountain streams to deep-sea adventures across the globe. He enjoys boating and adventure traveling with his family, experiences that he says allow him to “recharge and maintain clarity and creativity.” He also lives in Park City, Utah, where he enjoys skiing during the winter months.
Ultimately, Dr. Tettelbach’s entire approach can be distilled into his philosophy of servant leadership. “The foundation of effective leadership lies in humility, service, and empowering others to succeed,” he says. In a world of dazzling medical technology and big data, Dr. Tettelbach remains grounded in a simple, profound truth. He is optimistic that as more hospitals launch wound care clinics, they will realize the vast unmet need, and the specialty will grow organically. The best science, the best technology, and the best policies are all meaningless if we forget the person at the center of it all. His mission is to ensure that we never do, because when practiced appropriately, effective wound care will not only improve the quality of life for millions, but it will also extend life and mitigate a significant societal burden.
Quote
“The best care begins with listening.”
Also Read: 10 Most Impactful Wound Care Leaders to Watch in 2025